When Evidence Breaks
Rethinking Proof in the Age of Precision Medicine
Three exponentials are converging in medicine.
Diagnostics are expanding through genomics, proteomics, and molecular profiling, revealing fingerprints that once lay beyond human perception. Treatments are multiplying through computational chemistry, gene editing, and protein modeling systems like AlphaFold, each one tuned to strike ever narrower biological targets. Artificial intelligence now links these two worlds, matching diagnostic precision with therapeutic choice in real time.
This convergence does more than accelerate discovery. It challenges the foundations of evidence-based medicine itself. The more precisely we define a disease, the fewer people share it. Each refinement in diagnosis splinters the population into smaller groups, and each targeted therapy narrows its reach even further. What once applied to thousands now applies to hundreds, then dozens, then one.
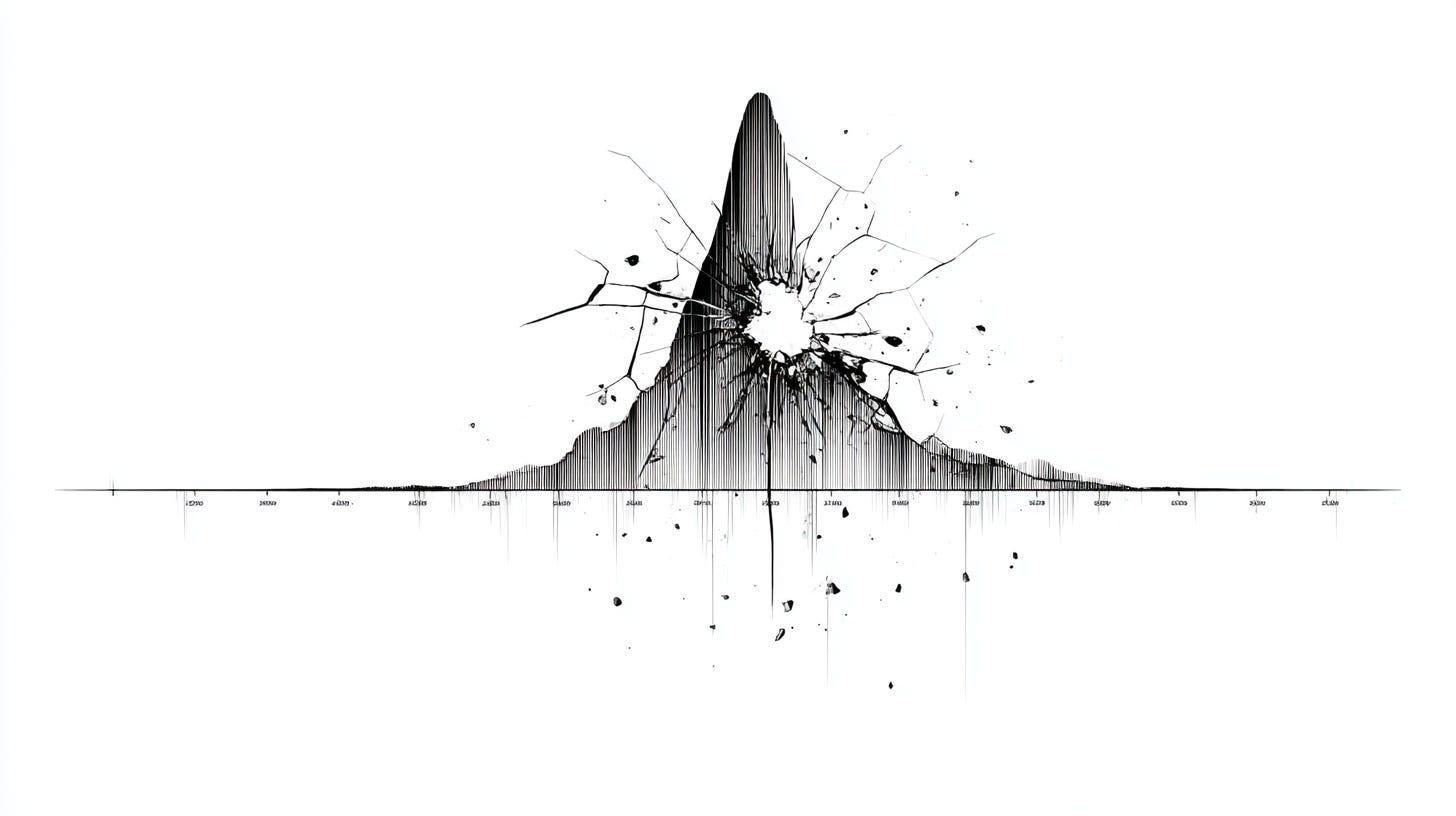
Evidence-based medicine was built on the logic of the average, on the power of large numbers to reveal universal truths. Precision medicine challenges that foundation. As the science becomes exact, the statistics fall apart. At the limit, medicine arrives where every patient is unique and every treatment must be proven anew.
The Collapse of the Average
The randomized controlled trial did not begin as dogma. It began as a breakthrough. In the mid-twentieth century, when medicine was wrestling with crude treatments and limited understanding, the RCT offered a way to separate real effects from illusion. Randomization eliminated bias. Control groups provided contrast. Averaging smoothed the noise of human variation into something that looked like truth.
It worked because the biology it measured was simple enough to permit it. Diseases were defined by symptoms, not genomes. Treatments were broad-spectrum by design: antibiotics that killed many bacteria, chemotherapies that struck any fast-dividing cell. The logic of the average fit a world built on similarity. If a therapy worked for most people most of the time, it was good medicine.
Over decades, the RCT became the gold standard not just for testing drugs but for defining what counted as knowledge itself. The method was rigorous, reproducible, and fair. It democratized discovery by making evidence collective.
But the very progress it enabled has begun to unmake it. As diagnostics fracture disease into finer molecular subtypes and treatments become tuned to genetic quirks, the cohorts that once filled a trial now dissolve into singularities. Variability is no longer the background to be averaged away; it is the entire story. The average patient, the invisible cornerstone of the RCT, has disappeared.
When the Denominator Is One
I learned the limits of evidence by living inside them.
My diagnosis was a rare form of multiple myeloma in which the malignant plasma cells are fewer but their byproducts more lethal. These cells release toxic misfolded proteins that deposit in organs such as the heart and kidneys. Over time they harden living tissue and erode its function. Once that process begins, the damage is hard to reverse. Getting treatment right the first time isn’t preference; it’s survival.
I began on the standard regimen, Daratumumab plus CyBorD, the frontline therapy that has transformed myeloma care. CyBorD, an older combination used across many cancers, hits the disease broadly; Daratumumab, an immunotherapy, changed the game by marking malignant plasma cells for immune attack. It worked at first, knocking the disease back, but after two cycles my response slowed. The standard advice was to stay the course. I wanted to know why.
Digging into the cytogenetics, I found the answer: a t(11;14) rearrangement, a variant that behaves differently from typical myeloma. In this subtype, the malignant plasma cells depend on a survival protein called BCL-2 to disable apoptosis, biology’s mechanism for removing defective cells. Venetoclax targets that vulnerability, blocking BCL-2 and restoring the cells’ ability to self-destruct.
That insight explained both the plateau and the next step. Daratumumab alone had mobilized the immune system but couldn’t overcome the cells’ internal resistance to death. Venetoclax could. Together, they addressed the cancer from two sides, immune and intrinsic. A phase 2 trial testing that pairing had already been approved, supported by both drug companies, but it was canceled when too few patients met the criteria. I decided not to wait for the next trial.
I proceeded anyway, off label, guided by mechanism rather than protocol. Daratumumab and Venetoclax together worked exactly as the biology predicted. The toxic proteins fell, my organ markers improved, and for the first time the treatment fit my actual biology rather than the average.
That is what it means when the denominator collapses to one. The framework of collective proof gives way to individual reasoning. The future of medicine will not always wait for statistical permission. Sometimes it has to act on understanding alone.
Three Exponentials, One Collision
Modern medicine no longer moves in straight lines. It evolves along three exponential curves that now feed each other faster than anyone can track.
The first is diagnostic power. We can now sequence an entire genome overnight, map the full proteome of a tumor, and read the molecular cross-talk inside its microenvironment. Each layer of analysis multiplies what we know. The patient stops being a case and becomes a dataset: millions of variables describing a single life. Every biopsy becomes a universe of information, expanding faster than any clinician can interpret unaided.
The second curve is therapeutic complexity. Once, cancer treatment relied on a few blunt tools: surgery, radiation, chemotherapy. Now its arsenal expands daily with monoclonal antibodies that enlist the immune system, CAR-T cells that hunt tumors, and small molecules engineered to fit a single mutation. Each new treatment defines its own subpopulation, dividing the field into ever smaller fractions.
The third curve is artificial intelligence, which is beginning to weave the others together. AI reads across modalities, learning from vast genomic datasets and clinical histories. It builds probabilistic models that see patterns no human can. It does not think in anecdotes or averages; it thinks in systems. It can integrate molecular biology, drug design, and clinical response in a single analytical frame.
I saw these forces converge in my own case. Using AI to analyze my bone marrow molecular profile, I mapped how my cytogenetics shaped the disease and pointed toward the treatment that best fit it. What once required an institutional research team could now unfold on a laptop.
When those three exponentials collide, the linear model of discovery disintegrates. The old cadence, form a hypothesis, design a trial, randomize, publish, built for a world of scarcity. Today the data arrive first and the hypotheses chase after them. Discovery happens continuously, in silico and in vivo at once. Each patient becomes both the experiment and the evidence.
The challenge is not producing knowledge but keeping up with it. The collision of these curves creates a living system that adapts faster than our institutions can validate. Medicine is shifting from a culture of delayed proof to one of real-time adaptation. The denominator keeps shrinking, but the intelligence that connects those fragments keeps expanding. That is where the next paradigm will form.
A New Paradigm for Proof
If the old gold standard was the randomized controlled trial, the new one must be continuous learning. Proof can no longer rest on static validation. In a world where every patient’s biology is distinct, waiting years for large trials to declare what works “on average” leaves too many behind. What we need now is a living system that adapts based on every case as it happens.
In this new paradigm, evidence is not a single verdict. It is an evolving process that absorbs diagnostic data, treatment paths, and outcomes from thousands of patients, then infers what is most likely to help the next one. Each experience, mine included, becomes both an individual success and a contribution to a shared intelligence. These stories are not anecdotes but the raw material of a continuously improving model of care.
Artificial intelligence makes this possible. It can find molecular and clinical similarities across populations too small for traditional trials, connecting patients who share a mutation, a pathway, or a treatment response invisible to the eye. It can calculate probabilities, suggest combinations, and refine its predictions with every new result.
Proof, in this context, becomes fluid. It no longer asks, “Does this work?” but “For whom, under what conditions, and with what degree of certainty right now?” The answer shifts as data grows. Certainty gives way to adaptability, and truth becomes something learned rather than declared.
Trust in this system will depend on transparency. We will need to see how models reason, which data they use, and how decisions evolve. Regulators will move from verifying outcomes to auditing learning systems. Fairness, provenance, and clarity will replace statistical finality as the marks of rigor.
The next standard of proof will not end with a publication. It will be medicine that evolves in real time, guided by every life it touches.
The Real Challenge
It’s tempting to see precision medicine as the next turn in a long scientific curve: better diagnostics reveal finer distinctions, leading to more targeted treatments. The pattern feels natural, even inevitable. Yet beneath that smooth progression lies a rupture. Once care becomes personal, the logic of evidence built on populations begins to collapse. Proof itself must change.
Evidence-based medicine arose in an age when commonality defined disease and scale defined truth. Its power came from repetition, the ability to show that a result held across many. Precision medicine reverses that premise. The more we uncover the molecular individuality of illness, the less those averages mean. The denominator that once made evidence strong now makes it brittle.
When the denominator becomes one, medicine shifts from a science of averages to a science of adaptation. Proof can’t rely on trials frozen in time; it must emerge from systems that learn continuously, updating their inferences as fast as understanding advances. Rigor will come not from uniformity but from responsiveness, from the capacity to explain and improve with each new case.
The challenge ahead is not discovery but definition. We must decide what “evidence-based” means when every case generates its own data and its own proof. The integrity of medicine will depend on how we rebuild that standard, one that honors individual precision without losing collective trust.