From Moon Landing to AI Landing
The Evolution of America's War on Cancer
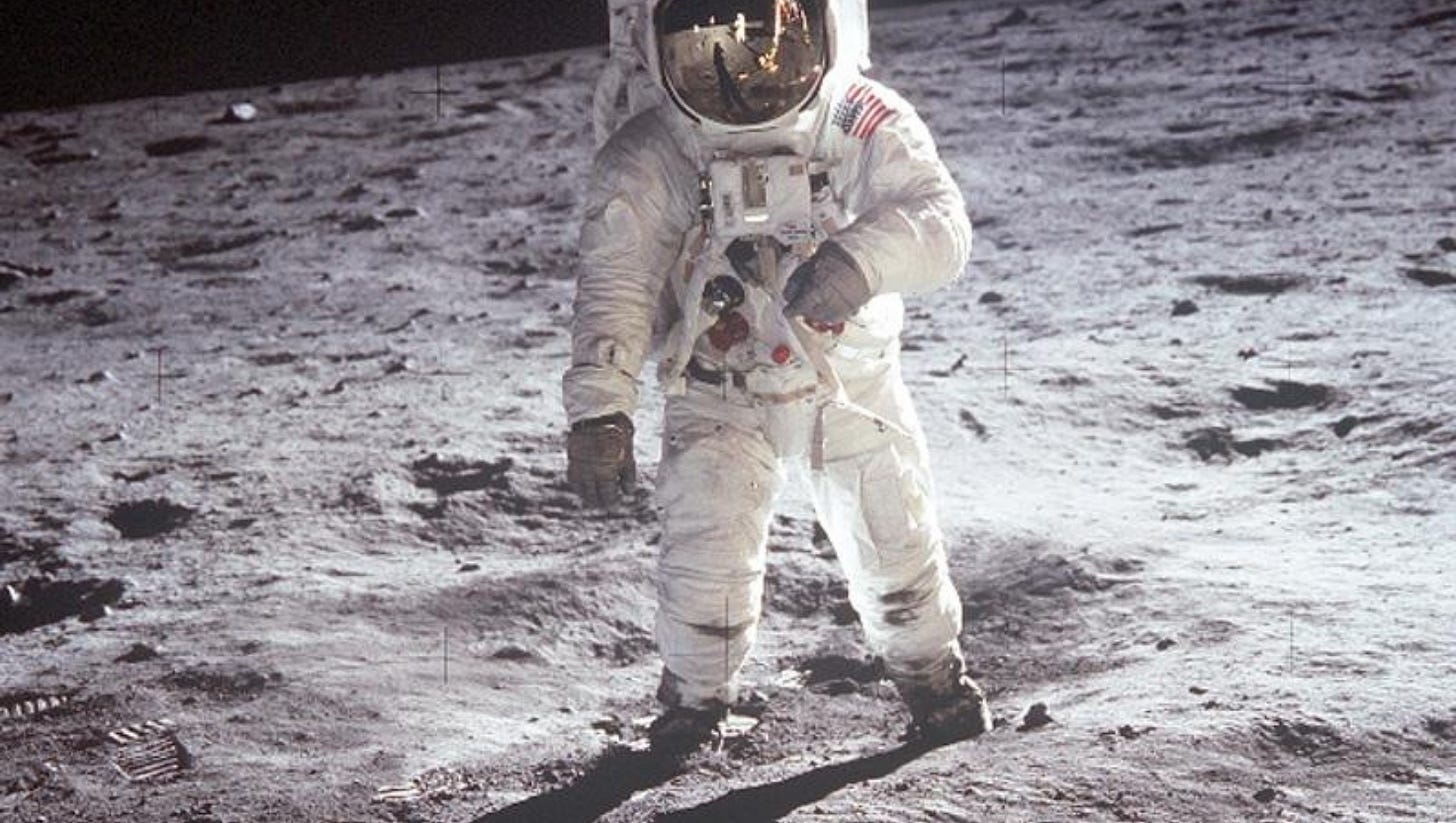
The Original Moonshot
On December 23, 1971, President Richard Nixon walked into the White House dining room with unusual ceremonial fanfare for a bill signing. Just two years after Americans had walked on the moon, he was about to launch what many called the original Cancer Moonshot—the National Cancer Act of 1971. With the stroke of his pen, Nixon declared an ambitious "war on cancer," promising that the same scientific prowess that had conquered space would soon conquer the disease that had become America's second leading cause of death.
The timing was no coincidence. Mary Lasker, the medical philanthropist who had tirelessly lobbied for this moment, understood the power of the moon landing metaphor. If America could put a man on the moon in less than a decade, surely it could cure cancer with equal determination and resources. The National Cancer Act allocated $1.6 billion and gave the National Cancer Institute unprecedented authority—its own budget procedures, a presidentially appointed director, and special status within the government.
The optimism was infectious. Scientists spoke confidently of eradicating cancer by America's bicentennial in 1976. The war metaphor dominated the language: we would carpet bomb tumors with chemotherapy, launch surgical strikes against malignant cells, and deploy radiation as our heavy artillery. Cancer was the enemy, and we would defeat it through sheer force and funding.
Moonshots Renewed
Nixon's moonshot was not the last. Nearly half a century later, the metaphor proved too powerful to abandon. In 2016, President Obama assigned Vice President Joe Biden to lead a new Cancer Moonshot, driven by personal tragedy—Biden's son Beau had died of brain cancer the year before. Obama tasked Biden with making "a decade's worth of advances in five years," doubling the rate of progress against cancer.
This modern moonshot differed from Nixon's brute-force approach. Where the 1971 effort had focused on massive funding increases, the 2016 initiative emphasized collaboration, data sharing, and breaking down silos between researchers. The 21st Century Cures Act provided $1.8 billion over seven years, but more importantly, it streamlined FDA approval processes and created new mechanisms for sharing cancer data across institutions.
Biden understood something Nixon's generation couldn't have: cancer wasn't just a research problem, but a data problem. The initiative launched Trials.Cancer.gov to help patients find clinical trials, created the Genomic Data Commons to share cancer genomics data, and focused on making federally funded research freely available to doctors and patients worldwide.
When Biden became president in 2021, he reignited the Cancer Moonshot with even bolder ambitions. The goal: cut cancer death rates by at least 50% over the next 25 years and prevent more than 4 million cancer deaths by 2047. His administration laid crucial groundwork—advancing ARPA-H, expanding data sharing, and investing in AI research infrastructure. But as political winds shifted and new administrations took office, it became clear that the next phase of cancer's defeat wouldn't come from Washington.
The Sobering Reality
Fifty-four years later, the scorecard is complex. We have not won the war on cancer in the sweeping victory that Nixon envisioned. Cancer remains the second leading cause of death in America, claiming over 600,000 lives annually. The disease has proven far more cunning, adaptive, and heterogeneous than the fixed target of the moon.
Yet the data tells a story of genuine, hard-fought progress. Since 1991, cancer death rates have declined steadily, averting over 4 million deaths. The age-adjusted cancer mortality rate has fallen by one-third since 1990, even as our population has grown larger and older. Childhood leukemias that were virtual death sentences in 1971 now have cure rates exceeding 90%. Five-year survival rates across all cancers have improved from 49% in the 1970s to nearly 70% today.
The original moonshot's most important legacy wasn't a cure—it was the infrastructure it created. The National Cancer Institute became a research powerhouse. The network of cancer centers it funded trained generations of oncologists. The investment in basic research laid the groundwork for every major breakthrough that followed: the discovery of oncogenes, the development of targeted therapies, the emergence of immunotherapy, and now, the AI revolution.
Why Cancer Proved Harder Than the Moon
The moon was a fixed target 240,000 miles away. Cancer is millions of different targets, each one evolving, adapting, and hiding within our own bodies. Every tumor is genetically unique—a fact that wasn't understood in 1971. Where Apollo required solving engineering problems with known physics, cancer required unraveling biological complexity that we're still discovering.
The early approach reflected this misunderstanding. Chemotherapy was indeed carpet bombing—flooding the body with toxic drugs that killed rapidly dividing cells, cancerous or not. Patients lost their hair, suffered devastating nausea, and endured profound weakness as the drugs attacked healthy cells alongside malignant ones. We were poisoning the whole body in hopes of poisoning the cancer just a little bit more.
But each failure taught us something. Each setback revealed new layers of cancer's complexity. The tumor that shrunk dramatically only to return months later taught us about drug resistance. The treatment that worked brilliantly in one patient but failed in another with seemingly identical cancer taught us about genetic heterogeneity. The cancer that vanished from scans but left behind invisible cells taught us about minimal residual disease.
The Precision Revolution
By the 1990s, our understanding had evolved dramatically. Cancer wasn't one disease but hundreds of different diseases, each with its own molecular signature. The Human Genome Project, completed in 2003, accelerated this insight. We began to understand that a KRAS-mutated lung cancer was biologically more similar to a KRAS-mutated colon cancer than it was to other lung cancers without that mutation.
This led to the precision medicine revolution. Instead of treating the organ where cancer appeared, we began treating the molecular disease itself. Drugs like Gleevec transformed certain leukemias from death sentences to manageable chronic conditions by targeting a single aberrant protein. Similar breakthroughs followed for lung cancers with EGFR mutations, melanomas with BRAF mutations, and breast cancers overexpressing HER2.
Immunotherapy represented an even more fundamental shift. Instead of trying to poison cancer cells, we learned to remove their invisibility cloak. Cancer cells survive by displaying molecular "don't eat me" signals that make them appear normal to the immune system. Checkpoint inhibitors strip away these false signals, allowing T-cells to see cancer for what it really is—a threat to be eliminated.
CAR-T cell therapy took this further, genetically engineering patients' own immune cells to recognize their cancer's specific fingerprint. The results have been miraculous for some patients—complete remissions in cases where all other treatments had failed.
Yet even with these advances, we still couldn't predict with certainty who would respond. Two patients with seemingly similar cancers could have completely different outcomes. The interaction between a unique cancer fingerprint, an individual immune system, and treatment involves thousands of variables beyond human comprehension.
Enter the AI Revolution
This is where artificial intelligence changes everything. We stand at another moonshot moment, but this time our rocket ship is made of algorithms, our fuel is data, and our destination is true personalized medicine.
The convergence is remarkable. Just as the original Cancer Moonshot benefited from 1960s advances in chemistry and radiation physics, today's battle against cancer benefits from 2020s advances in machine learning, computational power, and data availability. We now have the ability to sequence every gene in a tumor for under $1,000. We can monitor circulating tumor DNA in blood samples. We can analyze thousands of microscopic features in tissue samples. We generate massive amounts of data from every patient.
The problem is no longer generating data—it's making sense of it all. This is where AI excels. While human doctors can consider perhaps dozens of variables when making treatment decisions, AI can simultaneously analyze thousands of dimensions: complete genomic profiles, protein expression patterns, tumor microenvironment characteristics, immune system status, treatment histories from similar patients, and real-time monitoring data.
Recent breakthroughs demonstrate AI's transformative potential. Stanford Medicine's MUSK system combines medical images with clinical text to predict cancer prognoses and treatment responses with unprecedented accuracy. Harvard's CHIEF model performs multiple diagnostic tasks across 19 cancer types, achieving 94% accuracy in cancer detection while outperforming current AI approaches by up to 36%.
At the National Cancer Institute, AI algorithms now extract tumor features automatically from clinical text, saving thousands of hours of manual processing time. Large language models analyze vast medical literature, connecting insights from immunology papers in Japan with gene therapy trials in Boston and treatment protocols from Sweden.
The New Moonshot: N-of-1 Medicine
We're moving rapidly from treating cancer types, to treating molecular subtypes, to treating your cancer—singular, unique, with its own fingerprint and vulnerabilities. This is N-of-1 medicine: treatments designed specifically for your cancer's unique molecular signature.
AI makes this possible by recognizing patterns across thousands of dimensions that are invisible to human analysis. Where current medicine offers educated guesses based on population statistics, AI provides predictions based on deep pattern matching across vast molecular databases. Instead of saying "patients with your type of mutation usually respond to this drug," AI will predict "based on your complete genetic profile, tumor microenvironment, and immune status, combined with patterns learned from thousands of similar-but-not-identical cases, this specific combination of treatments has the highest probability of eliminating your unique cancer."
Companies like CureWise are building systems that turn cancer's overwhelming complexity into its downfall. Where doctors see bewildering arrays of mutations and biomarkers, AI sees patterns. Where traditional oncology offers treatment based on tumor location and a few biomarkers, these new systems analyze complete genomic profiles, tumor microenvironments, immune status, and treatment histories from thousands of similar cases to predict precise therapeutic combinations.
This isn't science fiction. Clinical trials are already underway using AI to match patients to optimal treatments, predict drug resistance before it occurs, and design combination therapies tailored to specific genetic profiles. Every patient treated with AI guidance teaches the system something new. Every unique cancer fingerprint analyzed reveals patterns that help the next patient.
This represents a fundamental shift from population medicine to truly personalized medicine. Instead of asking "what works for lung cancer patients?" we're asking "what will work for this patient's unique cancer?" The difference isn't academic—it's the difference between hope and certainty, between trial-and-error and surgical precision.
What's Different This Time
The original Cancer Moonshot was built on the reasonable but flawed assumption that cancer was a single enemy that could be defeated with sufficient force. Today's AI-powered approach recognizes cancer's true nature: not one disease but millions of different diseases, each requiring its own precise solution.
Several factors make the current moment uniquely promising:
Data Abundance: We now generate more cancer data in a single year than was accumulated in the first three decades of the war on cancer. This includes genomic data, imaging data, clinical outcomes data, and real-world evidence from electronic health records.
Computational Power: Modern AI systems can process and analyze datasets that would take human researchers lifetimes to review. Machine learning algorithms can detect patterns across thousands of variables simultaneously.
Understanding of Complexity: We now appreciate cancer's genetic diversity and evolutionary nature. Rather than fighting this complexity, AI embraces it, finding order within the chaos.
Speed of Discovery: AI accelerates every aspect of cancer research, from drug discovery to clinical trial design to treatment optimization. What once took years can now be accomplished in months or weeks.
Continuous Learning: Unlike the static approaches of the past, AI systems continuously improve. Every patient outcome feeds back into the system, making it smarter and more precise.
The Path Forward
The cure for cancer won't be a single breakthrough—it will be achieving such precision that we can eliminate each person's unique cancer cells as efficiently as a healthy immune system eliminates them naturally. AI is accelerating us toward this future faster than anyone imagined.
We're building systems that turn cancer's overwhelming complexity into its downfall. Where the original moonshot relied on brute force, the AI moonshot relies on surgical precision. Where Nixon's war on cancer fought the disease, today's approach partners with each patient's unique biology.
The moonshot metaphor remains apt, but the mission has evolved. We're no longer trying to reach a distant, fixed target. We're building a navigation system sophisticated enough to reach millions of different destinations—one for each patient's unique cancer. The rocket that will take us there isn't built of metal and fuel, but of algorithms and data, learning and adapting with each mission.
Fifty-four years after Nixon's declaration of war, we stand at the threshold of something even more ambitious: not just fighting cancer, but making it personally, precisely, and predictably curable. The moonshot continues, but this time, our destination is as unique as every patient we serve.
Three generations of presidential moonshots—Nixon's war of attrition, Obama and Biden's data-driven collaboration, and now the private sector's AI-powered precision campaign—each built on the failures and insights of the last. The political moonshots provided the foundation: Nixon's funding built the research infrastructure, Obama and Biden's initiatives broke down data silos and advanced collaboration. But the next phase belongs to entrepreneurs, technologists, and companies that can move at the speed of innovation rather than the pace of politics.
Cancer moonshots are no longer the exclusive domain of presidents and government agencies. They're happening in Silicon Valley startups, biotech companies, and AI labs where teams of engineers and oncologists are building the tools that will finally make cancer curable. Companies like CureWise represent this new generation—combining cutting-edge AI with deep medical expertise to create systems that can see patterns in cancer that no human mind could perceive.
Nixon's original moonshot promised to cure cancer by 1976. We missed that deadline by nearly half a century, but we learned something more valuable than any quick victory could have taught us: cancer's true nature and how to fight it. Every failure revealed new layers of complexity. Every breakthrough opened new possibilities. Every patient taught us something new.
The war on cancer isn't ending—it's evolving beyond the halls of government into the hands of innovators who can build, test, and deploy solutions in real-time. From the crude but necessary beginnings of chemotherapy to today's precision immunotherapies guided by artificial intelligence, we've traveled farther than any president could have imagined. The destination remains the same: a world where cancer becomes curable. But our route has become infinitely more sophisticated, traveling not through the vast emptiness of space, but through the dense landscape of human genetic diversity, guided by algorithms that can see patterns no human mind could perceive.
The next moonshot has already begun. This time, we're not just reaching for the stars—we're reaching for precision. And we're not waiting for Washington to show us the way.